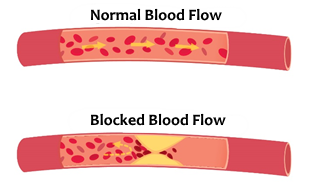
This is a chronic and asymptomatic process that begins at an early age. A layer of lipid plaque, muscle cells, white blood cells, etc. sinks between the inner layers of the arteries and narrows them.
Atherosclerosis becomes symptomatic as the plaque significantly constricts the artery and disrupts blood flow to the heart muscle.
When the heart does not receive the oxygen necessary for its activity, it will signal this deficiency through pain.
Factors
The causes of atherosclerosis are divided into controllable and uncontrollable factors:
Controllable: Smoking, proper nutrition, exercise, weight watching, mental stress, untreated diabetes, untreated high blood pressure.
Uncontrollable: age, gender (especially men) and heredity.
Prevention
So what can we do to prevent this?
- Eating healthy and in a balanced way
- Maintaining proper exercise (the recommended minimum is two hours of weekly sport)
- Following up with a doctor when over the age of 40 if there is a family history of heart disease
- Maintaining a calm lifestyle
An Israeli study of 25 to 45 year-olds found that maintaining a healthy breakfast lowers the lipid content levels in blood, reducing the likelihood of having a heart-related incident by half!
Angina Pectoris is known more commonly as chest pain.
These are chest pains caused by the process of atherosclerosis, which narrows the coronary arteries and as a result causes the heart to undergo ischemic (blood supply deficiency) processes.
- Stable Angina: A patient who complains of chest pain that is familiar to him and is felt during exertion (for example, after going up a staircase) and passing after rest. Most pains will be relieved with drug treatment.
- Unstable Angina: Chest pain related to the heart, unknown to the patient, appearing at rest and aggressive in nature, most often does not go away after drug treatment.
In all cases of chest pain, it is important to rush the patient to the hospital for fear that it is a complete obstruction of the coronary arteries requiring immediate treatment (myocardial infarction) or that the patient may need further clinical evaluation and supervision.
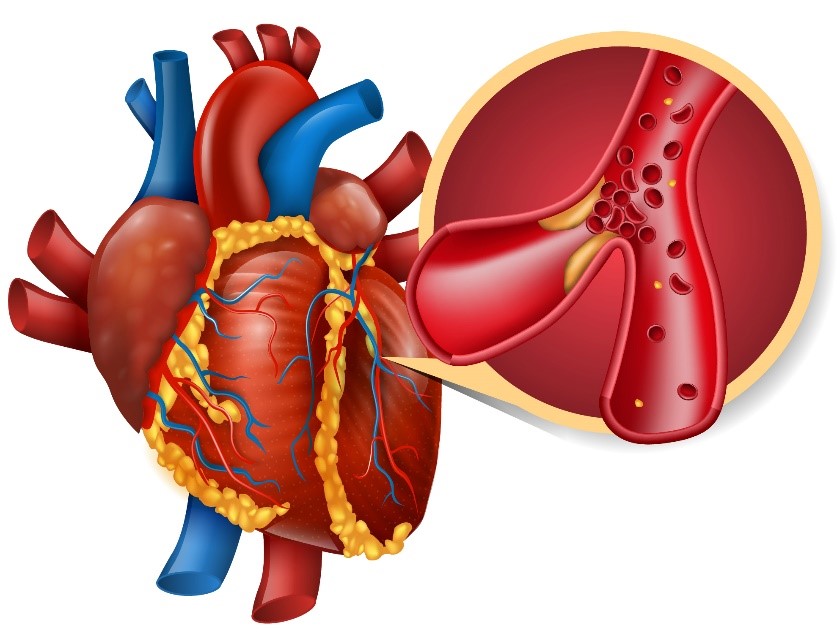
Complete blockage of a coronary artery that nourishes a segment of the heart.
In the field, we may suspect that this is a myocardial infarction based on the patient’s clinical signs and ECG examination.
In order to be able to diagnose accurately, we need to do a blood test that looks for specific substances that are only secreted when there is myocardial death, so we will always take the patient to the hospital to see if it is an infarction or other pain.
Arrhythmia (the most common cause of death from infarction), myocardial rupture, heart failure, pulmonary edema, cardiogenic shock.
Pay Attention!!!
It is a common mistake to think that a person having a heart attack will have a change in heart rate or must be unconscious.
During a heart attack, a patient is conscious and their heart rate can also be normal!
Myocardial infarction can be experienced without any chest pain, especially in diabetics, the elderly and alcoholics, who do not have properly functioning nervous systems.
The signs displayed, as mentioned, can be weakness, difficulty in breathing and paleness – so we need to increase vigilance, ask more questions and err on the side of safety so that we can suspect myocardial infarction by the patient’s appearance!
Cardiac arrest is a condition where the heart stops beating and as a result blood does not circulate throughout the body.
When we talk about cardiac arrest we always talk about mechanical cardiac arrest, although even when there is no mechanical heart activity this does not mean there is no electrical activity. Cardiac arrest and severe arrhythmia will not allow adequate blood circulation to the body.
- Cardiac arrest (Asystole) – The term refers to the mechanical activity of the heart, but it is a cardiac arrest in which there is no electrical activity as well as no mechanical activity.
- Ventricular fibrillation (VF) – a condition in which the ventricles contract rapidly, arrythmically (with electrical activity) and are ineffective (the heart is unable to contract effectively and pump blood into the body).
- Pulseless Ventricular Tachycardia – As the name implies, there is rapid electrical activity in the heart but it cannot contract mechanically.
- Pulseless Electrical Activity-PEA – A condition where the heart has no mechanical activity (does not contract), but when the patient is connected to an ECG you can see slight and inadequate electrical activity.
When we connect a patient to a defibrillator during CPR, we want to see if providing a shock from the defibrillator resets the heart’s electrical activity (creating asystole) and allows it to return to its normal pace.
Treatment
The treatment for these conditions is CPR and calling an ambulance.
During cardiac arrest and PEA the defibrillator will not recommend providing a shock as cardiac activity is already reset in these situations.
A chronic condition caused by death or injury to heart tissue.
Let’s imagine the heart’s activity as a bucket being filled by a cup; normally the cup will take a fixed amount of water every time it is emptied into the bucket. Heart failure is a condition where there is a hole in the cup. Now the cup will not transfer the same amount of water as it loses water on its way to the bucket. Thus the heart is not able to pump the same amount of blood as it used to.
Due to a lack of forward blood circulation (to the body), blood accumulates in the chest area and the fluid from the blood escapes to the lungs. This is called a “pulmonary edema” and is a life-threatening condition.
- Breathing problems
- Paleness and cold sweat – signs of adrenaline secretion due to the body’s distress
- Rapid heartbeat
Deterioration can be extremely rapid.